Dive Brief:
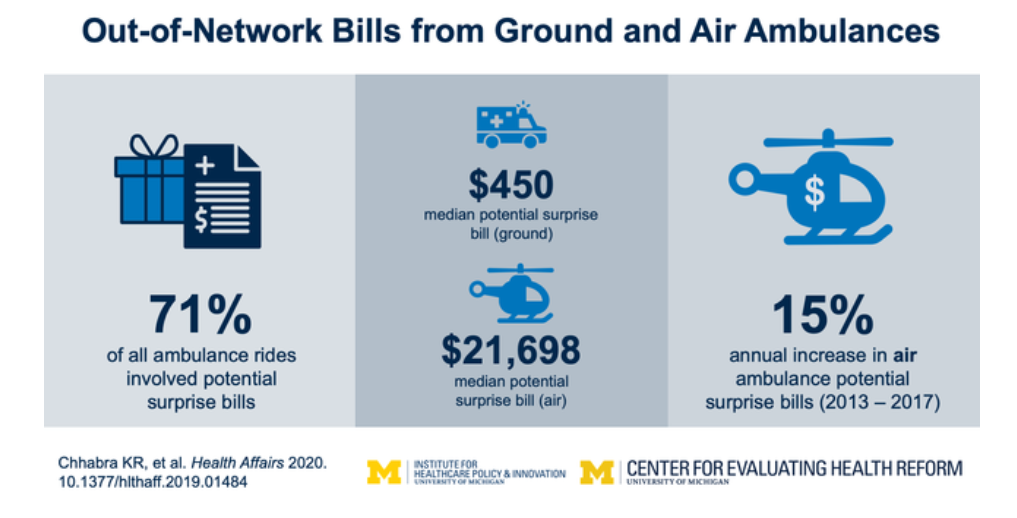
- More than 70% of air and ground ambulance rides taken by members of a major commercial insurer between 2013 and 2017 involved a potential surprise bill, according to a study published Wednesday in Health Affairs.
- The amount billed to a patient was substantially higher for air ambulance services at a median of nearly $ 21,700, but ground ambulance rides were more likely to invoke a possible surprise out-of-network bill and had a larger aggregate impact of about $ 129 million per year.
- A separate study published simultaneously in Health Affairs found that about 8% of services at in-network ambulatory surgery centers had a potential for a surprise bill, with anesthesiologists generating the most at 44%, followed by nurse anesthetists at 25% and independent laboratories at 10%.
Dive Insight:
Surprise billing was in the health policy spotlight toward the end of last year. While the COVID-19 pandemic has certainly overwhelmed the U.S. health system and lawmakers attempting to restart a halted economy, the idea of banning the practice has been discussed in legislation addressing the crisis.
In the Coronavirus Aid, Relief, and Economic Security Act passed late last month, Congress allocated $ 100 billion to hospitals to help them treat and prepare for patients infected with the novel coronavirus. As CMS distributed the first $ 30 billion at the end of last week, officials stipulated providers accepting the money would not be allowed to surprise bill those patients.
And legislative debates for that bill and subsequent emergency relief have considered more broad language attempting to curb surprise bills. Despite bipartisan consensus that the patients should be held harmless when they are unwittingly treated by an out-of-network provider at an in-network facility, lawmakers have so far been unable to reach an agreement for how to settle those payments as hospital and insurer lobbies spent heavily for their favored policies.
The economic downturn expected as the economy crashes amid the public health emergency and millions file for unemployment could bring more attention to the issue. Already, there are several media reports of people who received unexpected bills for COVID-19 testing and treatment.
The Health Affairs report looking at surprise billing at ASCs found the size of the charges increased 81% over the the four years studied, reaching an average of $ 1,483 in 2017. That research used Health Care Cost Institute data from patients in UnitedHealth Group, Humana and Aetna commercial plans.
The ambulance ride paper notes air ambulance charges increased rapidly between 2013 and 2017 despite an increase in bases and providers that would be expected to increase competition and decrease prices.
“The air ambulance business model’s favorable economics have led to rapid investment by for-profit and private equity–owned firms, with additional capacity being added in regions that already have air medical coverage,” the authors wrote. “Aggressive price increases coupled with limited network participation and supply-driven overuse may be contributing to the growth in aggressive billing from air ambulances.”
